Bariatric surgery refers to surgical procedures which reduce the weight of severely overweight patients. They include gastric bypass, sleeve gastrectomy or gastric band. Depending on the procedure, either the stomach is reduced in size or food is diverted past the stomach.
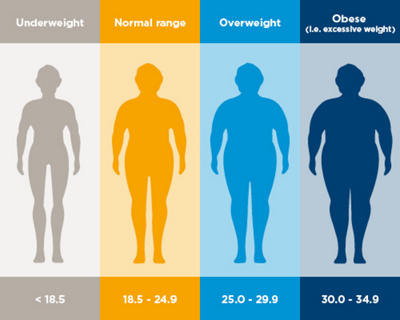
If a person has a body mass index of more than 30, they are deemed to be severely overweight or obese. Patients with a BMI of more 30 can often not keep weight off despite going on a diet. Surgical procedures can therefore lead to long-term weight reduction. According to the latest studies, obese patients with diabetes will gain particular benefit from obesity surgery.
Depending on the situation, different surgical methods can be employed to reduce the patient's weight. The main principle of the operation is either to achieve an early feeling of fullness or to reduce the food intake.
What preparations are carried out before the procedure?
Different clarifications and examinations are undertaken before the procedure. This includes a blood test, x-ray and ultrasound examinations, as well as an ECG, blood pressure measurement and, if necessary, a gastroscopy.
All blood-thinning medication must be discontinued prior to surgery. The operation is performed under general anaesthetic. Patients should therefore be fasting for the procedure.
How is the operation performed?
The choice of surgical method is determined by every patient's individual situation. Nowadays gastric bypass and sleeve gastrectomy are the most common procedures for obese patients. Gastric bands are only used in exceptional circumstances.
Nowadays all procedures are usually carried out laparoscopically. This minimally invasive procedure involves inserting a video camera and surgical instruments into the abdominal cavity via several small incisions in the skin.
Gastric bypass
A gastric bypass is the most common operation for patients who are severely overweight. In the process, the stomach is severed and sutured together shortly after the juncture of the oesophagus. The remaining small abdominal pocket is directly connected to the small bowel. Food is directed past the stomach to a part of the small bowel. Depending on the length of the piece of the small bowel which has to be bridged, the surgery is referred to as a proximal (short) or distal (long) gastric bypass. This operation has a dual effect on food intake: Initially only smaller meals can be consumed and the patient feels full earlier. Secondly, less food is actually digested as a part of the small bowel is completely shut down. However, this can actually reduce the intake of certain vitamins and minerals as well. Therefore, the requisite preparations need to be taken to prevent symptoms of deficiency.
Sleeve gastrectomy
Sleeve gastrectomy is a relatively new operation method. During this procedure, the stomach is reduced to the size of a sleeve. Around 80% of the stomach is removed. In the process, a percentage of the stomach which stimulates the "hunger hormone" Ghrelin is also taken out. As a result, patients feel less hungry. The reduction in the size of their stomach quickly leads in turn to a feeling of fullness.
Biliopancreatic diversion
Biliopancreatic diversion is a method by which the reduction in the size of the stomach is combined with a bypass of the small bowel. In comparison to gastric bypass surgery, a much longer section of the small bowel is bypassed. As a result, the bowel, which is available for digestion and food intake, is markedly shortened. This leads to significant weight loss. However, the complication rates for this procedure and the risk of deficiency symptoms are higher. The operation is therefore only used on patients who are extremely overweight, and when other methods are inadequate.
Gastric band
Gastric band surgery involves laying a plastic sleeve made of silicone under the junction of the oesophagus around the stomach. The resulting constriction of the stomach means the patient can consume less food. The sleeve is connected to a fluid reservoir which is implanted under the skin. This means that the constriction of the stomach can be regulated outside the body.
In earlier times, a gastric band was the most common procedure for obese patients. More effective procedures such as gastric bypass or sleeve stomach, which have fewer long-term complications, have made this method more or less unnecessary.
What is the success rate of this procedure?
Gastric bypass and sleeve gastrectomy have a similarly good effect on weight reduction. The patient's weight usually drops by around 60% within 5 years of the surgery. As the sleeve gastrectomy method is newer, there is still no literature documenting its long-term effectiveness.
What are the possible complications and risks of this procedure?
As with all surgery, this operation may occasionally lead to post-operative haemorrhaging, nerve damage or infections. Artificial connections with the small bowel can sometimes not work properly. Patients who undergo gastric band surgery may suffer complications years later which make it necessary to remove the band. Shutting off a part of the natural digestive tract can lead to digestive disorders and deficiency symptoms.
What happens after the operation?
The food intake must be increased slowly and carefully after bariatric surgery. The body must accustom itself to the changed conditions in the digestive tract. At the beginning, upper abdominal complaints such as a feeling of fullness or nausea may occur. The food often reaches the colon too quickly due to bypassing the stomach. This can lead to an increase in blood sugar or diarrhoea. The patient's eating habits should be adjusted to these changed conditions: Smaller portions several times per day. No meals consisting solely of carbohydrates. Do not drink immediately before and during the meal.
Depending on the situation, vitamins and trace elements are required to prevent symptoms of deficiency. Long-term weight reduction is dependent on the patient undergoing regular checks and adhering consistently to the after-care.

