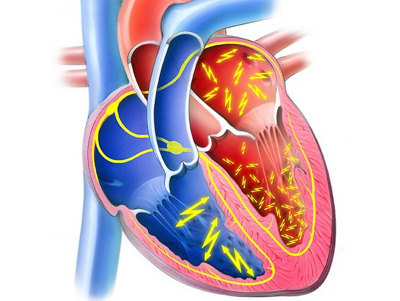
Atrial fibrillation is one of the most common heart rhythm disorders and it mainly occurs in old age. The heartbeat becomes irregular, because the atriums and the ventricles beat at different rates. Atrial fibrillation treatments are designed to prevent strokes, improve quality of life and avoid the long-term development of cardiac insufficiency.
Treatment of atrial fibrillation aims to restore what is known as a sinus rhythm. Although there are no studies indicating that a sinus rhythm is better than atrial fibrillation with regard to mortality or complications, patients obviously find it more comfortable to have a sinus rhythm. They feel better, do not have any symptoms and their heart reacts appropriately to physical exertion and emotional responses.
Top priority: stroke prevention
The main aim of any atrial fibrillation treatment is to prevent a stroke. Doctors therefore seek to control the rhythm of the heartbeat. This means restoring a sinus rhythm, minimising symptoms, preventing complications and possibly enabling the patient to stop using blood thinning medication.
Untreated atrial fibrillation is responsible for around 15 percent of all stokes. There are various medications available for controlling the heartbeat’s frequency or rhythm – they are known as antiarrhythmic agents. However, they are not without side effects and often cannot prevent the disorder from returning.
The choice of treatment options always depends on the patient’s individual case: Is the atrial fibrillation paroxysmal or not? Does the patient suffer from any other heart diseases? These factors will determine which electrophysiological or surgical methods are used.
Ablation – Immobilising certain tissues in the heart
During an ablation procedure, the tissue responsible for the uncontrolled electrical heart activity is eliminated. This is achieved surgically with a scalpel or electrophysiologically using a catheter (through which radiofrequency waves or cold, i.e. cryotherapy, is applied). Scars are created to immobilise or isolate certain parts of the heart tissue.
In the case of catheter ablation, a catheter is inserted via an artery in the groin and pushed through to the heart, where it is then used to create scar tissue (ablations) in the right atrium. If the source of the atrial fibrillation is in the left atrium, it is much more difficult to access with a catheter.
Heart surgery – Accessing the heart using the keyhole technique
Surgical ablation used to be performed during open heart surgery. The patient would be attached to a heart-lung machine and the tissue responsible for the atrial fibrillation would literally be removed from the heart. Known as the ‘maze procedure’, this method was very successful in terms of fixing the atrial fibrillation, but it was of course also associated with significant complications and other adverse side effects.
Today the same result is achieved using keyhole surgery, whereby the heart is accessed via three small incisions to the left and right. This means the patient no longer needs to be attached to a heart-lung machine.
The method is ideal for treating atrial fibrillation. For patients suffering from paroxysmal atrial fibrillation, this technique is used to isolate the pulmonary arteries outside the heart. The recently published FAST study (Boersma et al. Circulation. 2012 Jan 3;125(1):23-30.) revealed that this surgical procedure delivered a success rate of over 70 percent after one year in patients with an enlarged left atrium or who had already had a catheter ablation. By comparison, the success rate of catheter ablations in the same patient group is around 40 percent.
In our experience the results are even better. After a patient with paroxysmal atrial fibrillation has undergone one thoracoscopic ablation procedure, we anticipate a success rate of well over 90%. During the thoracoscopic procedure the heart’s left auricle is also disabled by means of stapling and as a result the patient is able to stop using blood thinning medication – regardless of their heart rhythm. Patients benefit from an extremely high level of safety and increased quality of life.
Stroke prevention – Using blood thinning medication
The risk of a stroke is determined using the CHADS-VASC table, in which different risk factors are assigned a certain number of points. For instance, high blood pressure is worth one point, being aged over 75 is two points, diabetes is one point, etc. Anyone with a total of two points or more should definitely receive stroke prevention treatment, i.e. blood thinning medication.
But in practice, studies have shown that patients with atrial fibrillation often do not receive sufficient stroke prevention (blood thinners). These studies relate to blood thinning by means of vitamin K antagonists, which are relatively difficult to stop using and have to be monitored regularly (Quick). Consequently new blood thinners have been developed that are easier to use and monitor, although long-term studies about these new products are not yet available.
Another risk factor table known as HAS-BLED helps doctors to determine the risk of haemorrhaging in patients required to take blood thinning medication. In practice, the risk of a stroke (CHADS-VASC table) is therefore always weighed up against the risk of haemorrhaging (HAS-BLED table).
Alternatives to blood thinners
Clots that cause vascular blockages are formed in the heart’s left auricle, so strokes can be avoided by either surgically removing the left auricle or sealing it with a device called an ‘umbrella’. This operation is particularly advisable if the patient has suffered complications caused by blood thinners or cannot take blood thinning medication. The left auricle is especially important for young, sporty people, because it acts like a turbo engine or an additional back-up pump during physically demanding activities. Given the potential complications, older people can afford to lose an auricle.
The auricle comes in a variety of different forms. It can be shaped like a cauliflower, cactus, chicken wing or wind sock. An interesting US study (Di Base et al. J Am Coll Cardiol. 2012 Aug 7;60(6):531-8) has shown that a person’s risk of stroke is related to the shape of their auricle. People with an auricle like a chicken wing are the least likely to have a stroke, while people with cactus or cauliflower-shaped auricles face the greatest risk. So not all heart auricles are equally dangerous.
Did you miss the first part of this blog post? You can read it here: Atrial fibrillation (part 1 of 2) – When the heart loses its rhythm.
More information about cardiovascular health and heart surgery is available from Heart Clinic Hirslanden.
